Medical Case Management
- Field and Telephonic Case Management
- Coordinate IME’s, 2nd Opinions,
Diagnostic Testing - Assist Employer to Develop & Identify Modified Duty Work Programs
- Workers’ Compensation Provider Panels
- Cost Projection & Savings
- File Review
- Catastrophic
Clinical Areas of Expertise
- Major Trauma - Falls, Motor Vehicle Accidents
- Catastrophic Injury
- Traumatic Brain / Spinal Cord
- Burns
- Amputation
- Orthopedic
- Chronic Pain
- Wound Care
- Discharge Planning & Coordination
- Pulmonary Illness
- Mobility Assistance
- Concussion

Case management is a collaborative process that assesses, plans, coordinates and evaluates the options and services required to meet the injured worker’s health and medical needs. It is characterized by advocacy, communication and resource management and promotes quality and cost-effective interventions and outcomes.
Early and aggressive medical intervention, along with the appropriate allocation of clinical resources, can significantly improve workers compensation lost costs, the cost of lost wages, productivity and medical expenses.
Value of Case Management Intervention:
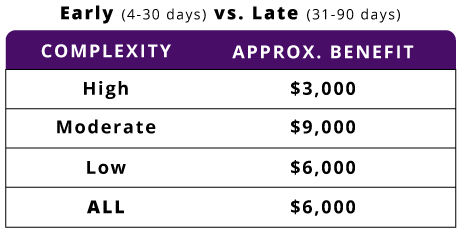
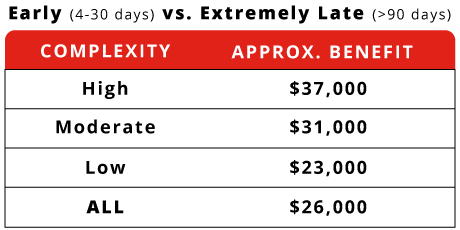
Zurick’s Analysis of nearly 28,000 claims showed that the timing of nurse case manager referral can have significant impact on the total cost of a claim as well as the closing rate.
The analysis looked at three distinct referral time frames:
- Early: 4-30 days
- Late: 31-90 days
- Extremely late: After 90 days
Ultimately, the analysis confirmed longstanding belief: Early referral claims is optimal
When nurses are engaged early, the result can be an average $6,000-$26,000 total savings per claim, with nearly 50% of that savings in medical spend.
Early Nurse Case Management Referral Benefit
Early implementation of case management to claims have reduced disability days by as much as 30% and close 20% quicker.
PCMS nurse case managers are critical links between injured workers, their families, physicians, employers and insurance companies. Working collaboratively with all involved parties, our case managers help establish the best plan of care and provide clinical oversight to help injured employees return to work as quickly and safely as possible.

